Have you ever bought a drug and later found out you couldn’t use it, maybe because you’re pregnant, breastfeeding, or you have an ulcer?
Not every medicine you see on the shelf is safe for everyone — even if it doesn’t require a prescription.
As a pharmacist, here are 5 things I advise you to always check before picking any medication.
CHECK THE EXPIRY DATE
Expired medicines can lose potency or even become harmful. That “small date” can make a big difference to your health. Always check the expiry before paying.
Most people confuse expiry date, best before, and use by, especially on medicines, supplements, and even some health foods.
What’s the difference between these terms?
EXPIRY DATE
This is the last date the manufacturer guarantees the full safety and strength of the product.
It may be written as DD/MM/YY, but sometimes only the month and year may be recorded. In this case, the expiry date is the LAST DAY of that month.
For example, if expiry is October 2025, the medication should not be used after 31st October, 2025.
After this date, the medicine may not work properly or could become unsafe.
Never use a drug after its expiry date even if it looks fine
SIGNS OF EXPIRY
Changes in color, texture, or smell, such as pills crumbling or liquids becoming cloudy.
You should also check for mold, spots, swelling, or clumps in pills.
Look for particles or discoloration in liquid medications, especially injectables.
BEST BEFORE
It tells you how long the product will retain its best quality: taste, texture, potency.
Sometimes, you can often use it after this date, but it might not be at its best.
USE BY
Found on perishable or sensitive health products — like certain probiotics, baby formulas, or eye drops.
This date means do not use after this point for safety reasons.
For example, Eye drops are to be used by ONE MONTH AFTER OPENING, NO MATTER THE EXPIRY DATE.
An eye drop may have an expiry date of January 2028. However, if it is opened on the 21st of October 2025, it MUST BE USED BY 21st November 2025, and then discarded even if the bottle isn’t empty.
Using it beyond this date is dangerous.
CHECK THE ACTIVE INGREDIENT
Different brands often contain the same drug. For example:
Panadol = Paracetamol
Emzor Paracetamol = Paracetamol
Tylenol = Paracetamol
Taking both means you’re double-dosing unknowingly.
Always look at the active ingredient, not just the brand name. If you’re not sure, ask the pharmacist.
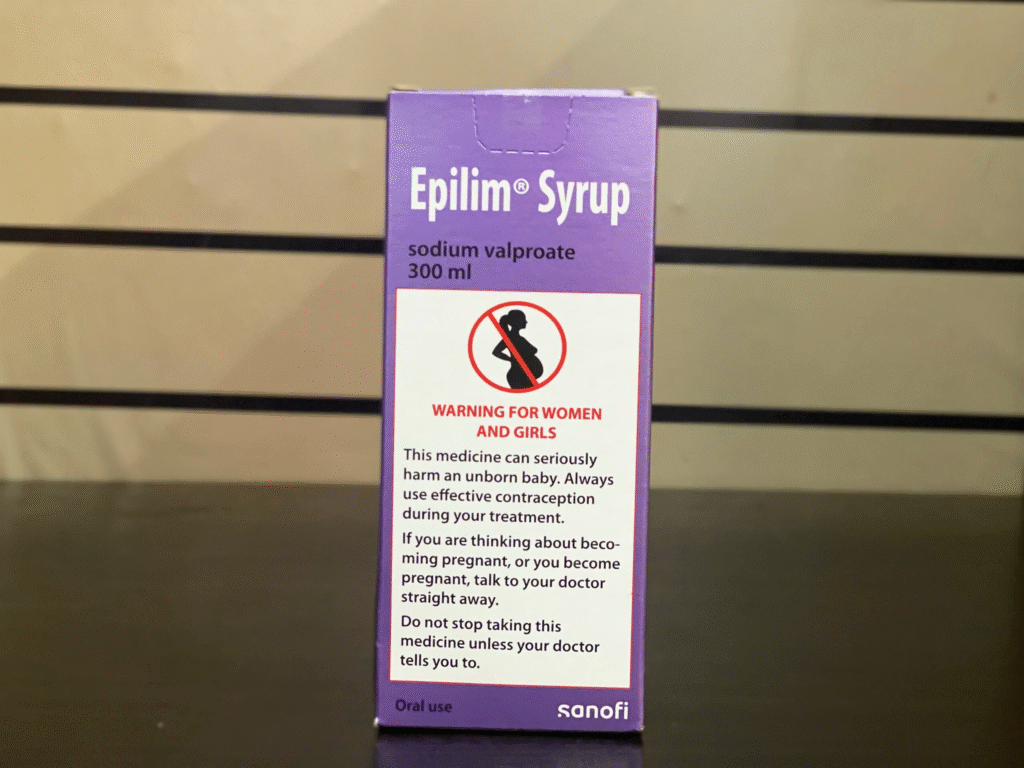
CHECK THE DOSAGE AND INSTRUCTIONS
The label tells you how much, how often, and who can take it.
Some drugs aren’t safe for children, pregnant women, or people with high blood pressure, ulcers, or asthma.
⚠️ Look out for warning signs on the package. What works for one person may harm another.
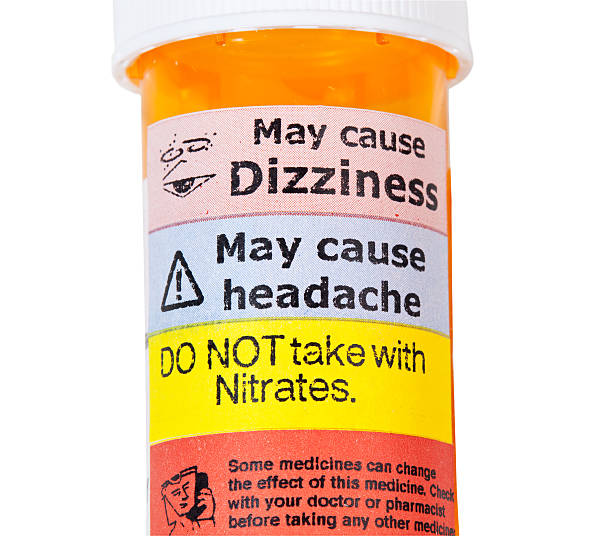
CHECK FOR INTERACTIONS AND SIDE EFFECTS
Some OTC (over-the-counter) drugs can interact with your current medicines or supplements.
For example:
Painkillers like ibuprofen and diclofenac can irritate ulcers.
Antihistamines (like Chlorpheniramine, comonly called Piriton, and diphenhydramine) common in cough syrups and cold meds can cause drowsiness.
Herbal supplements can interfere with prescription drugs.
If you’re taking any regular medication, always ask a pharmacist first.
CHECK THE PACKAGING AND SEAL
Broken seals, faded print, or repackaged tablets? DO NOT USE!
They could be counterfeit or poorly stored.
Only buy medicines that are sealed, clearly labeled, and from licensed pharmacies.
OTC doesn’t mean risk-free.
A 30-second check can prevent wrong doses, drug interactions, and side effects.
If you’re ever unsure, ask your pharmacist. That’s what we’re here for — to keep you safe.
Source Credit: Originally posted on X (Twitter) by @EfthaliaCare